Abstract
Background: Since 2019, Community Voices in Research (CVR), a community-powered registry supported by the National Hemophilia Foundation, collects information directly from persons with inheritable bleeding disorders (IBDs) (PWIBD) and their immediate family members aiming to understand their lived experiences. The self-reported, de-identified, aggregate data are used to improve clinical outcomes and quality of life for PWIBD and identify research questions important to the community. The aim of this analysis was to describe the relationship between self-reported mental health (MH) diagnosis, history of MH treatment, participation in physical activity (PA), chronic pain, and social support.
Methods: Participants voluntarily enrolled and completed the surveys. Surveys include self-reported information such as socio-demographics, IBD diagnosis, comorbidities, treatment, pain, PA level, MH, and social support - validated tools were used for the last two.
Data were analyzed using Stata 15.1. Chi square and Fisher's Exact tests (the latter if n in any cell was <10) were used for frequency count (categorical) data, Spearman's Rho was used for correlational analysis of rank order data, t tests for unequal variances were used for non-normally distributed interval level data, and Kruskal-Wallis equality of proportions tests were used to compare groups on rank ordered or highly skewed interval level data.
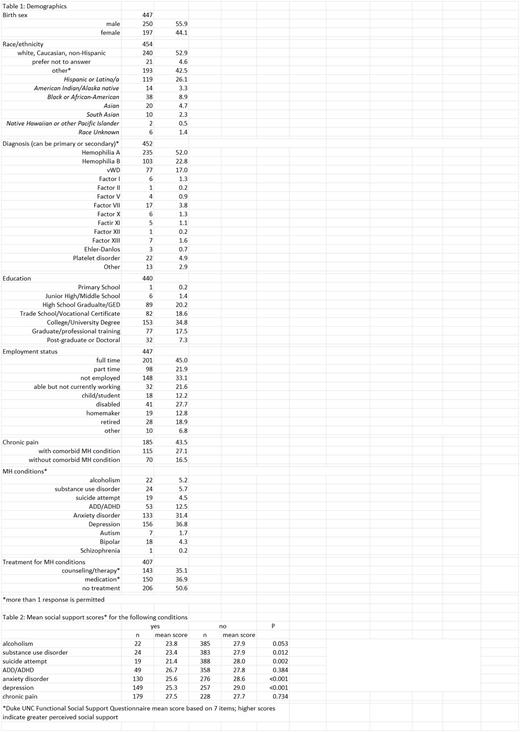
Results: Respondents with an IBD completed both the enrollment survey and at least part of the baseline survey (n=456). Variable response numbers for specific analyses range from 407 to 447 due to survey logic and incomplete baseline surveys. Table 1 describes sociodemographic characteristics.
When compared to male respondents, females were more likely to have history of anxiety (45.5% vs. 20.3%, P<0.001), depression (48.7% vs. 27.4%, P<0.001), bipolar disorder (7.5% vs. 1.7%, P=0.006), and autism (3.2% vs. 0.4%, P=0.047) and did not differ significantly (P>0.10) from males in percentages of alcoholism (5.9% vs. 4.6%), substance use disorder (7.5% vs. 4.2%), ADD/ADHD (15.5% vs. 10.1%, or schizophrenia (0% vs. 0.4%). Due to the low rates of bipolar disorder, autism, and schizophrenia in the sample, these MH conditions were not evaluated further beyond inclusion in bivariate analyses comparing those with and without a MH condition.
Those who did not engage in PA (n=45/11.1%) were compared with those who engaged in at least one PA (n=362/88.9%); inactive respondents had higher scores for depression (58.4 vs 53.4, P=0.008) and anxiety (16.7 vs. 14.3, P=0.031). History of counseling/therapy, medication, or no treatment for a MH condition did not differ significantly by gender, nor did current depression, anxiety, or social support scores (all with P>0.10). Education level and employment status (full time, part time, unemployed) were not associated with treatment vs. no treatment for any MH condition (all with P>0.07). The majority of those with a MH condition had at least one additional comorbid MH condition, ranging from 75.5% for those with ADD/ADHD to 100% for those with history of suicide attempt. The majority of those with chronic pain (85.6%) had a comorbid MH condition.
At least one past or current MH condition was present in 216 (50.8%) of respondents and was associated with less perceived social support, either with (n=115/53.2%) or without (101/46.8%) comorbid chronic pain (P<0.001). Those with chronic pain and no MH condition (n=68/16%) had the highest perceived social support while those with a MH condition in the absence of chronic pain (n=97/22.8%) had the lowest. Those with history of alcoholism, substance use disorder, suicide attempt, anxiety, disorder, and depression all had less perceived social support than those without these conditions (Table 2). Current depression and anxiety scores were inversely correlated with perceived social support (Rho=-602 and -0.506 respectively, P<0.001).
Conclusions: PWIBD with self-reported MH conditions had at least 1 MH comorbidity, report a lack of perceived social support and were less physically active than PWIBD without a self-reported MH condition. Patient advocacy organizations and treatment centers can use this information to develop resources to help this population. Research is needed to further describe these relationships.
Disclosures
Santaella:National Hemophilia Foundation: Current Employment. Nichols:National Hemophilia Foundation: Current Employment. Carlson:National Hemophilia Foundation: Current Employment. Witkop:National Hemophilia Foundation: Current Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal